By Kim Yu, MD, FAAFP
kyu@aledade.com
National Director, Clinical and Community Partnerships, Aledade
President, Orange County Chapter, CAFP
What is Value-Based Care and What Does it Mean for Family Physicians in Primary Care?
Value-based care is the concept that physicians should be reimbursed based on patient outcomes instead of the volume of services provided. The goal is to help individuals maintain their highest possible level of wellness rather than waiting to provide care until patients get sick, which is often a more complex and expensive task. In value-based care arrangements, practices, clinics, community health centers (CHCs) and other primary care organizations contract with payers, such as Medicare, Medicaid, and commercial insurance companies, to care for a defined set of attributed patients.
To earn financial rewards, physicians must meet specific performance and quality measures that are tied to better long-term outcomes for patients. These measures may include the delivery of routine and preventive care services and chronic disease management services. By prioritizing quality over quantity, value-based care can help to make healthcare more efficient and effective for patients, physicians, and payers.
How does value-based care work?
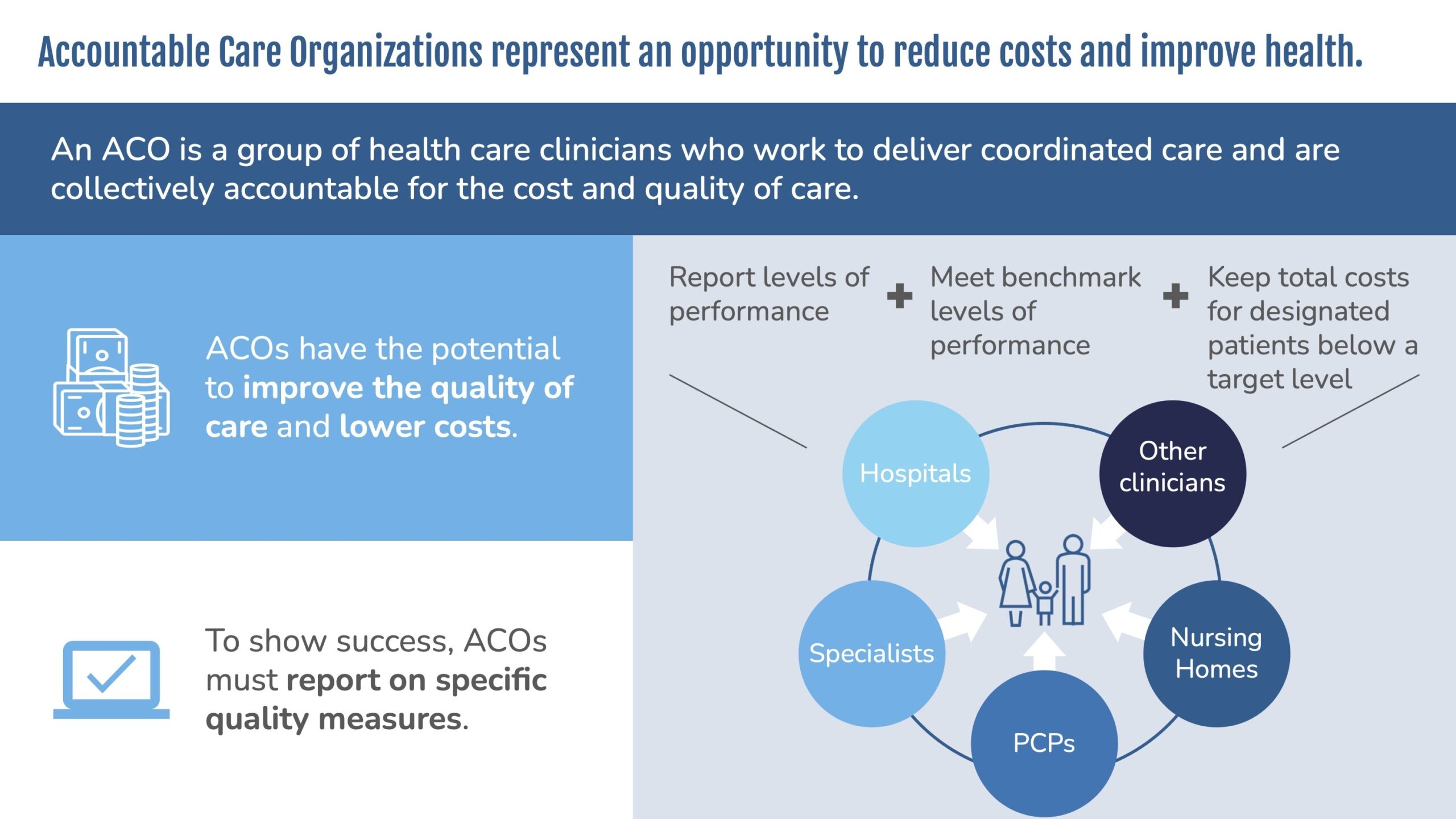
Value-based care impacts every piece of the healthcare process, from the back office and the waiting area to the exam room and even the patient’s own home. To implement the necessary changes in a sustainable way, physicians can work together within accountable care organizations (ACOs), which are groups of physicians, hospitals, and other clinicians jointly responsible for managing an attributed population. ACOs create a structured framework for tackling the two major components of value-based care: accepting financial risk and improving care management.
What about financial risk?
The biggest difference between value-based care and fee-for-service is the idea of incorporating financial risk into care delivery. ACOs offer a flexible way to incentivize physicians and improve quality in partnership with payers. If an ACO meets its quality goals and spending benchmarks, it could receive a portion of the savings, or the difference between what the payer expected to spend on care for the attributed population and the actual spending for the performance period.
Many ACOs choose to participate in upside-only risk models, meaning that they receive shared savings if they succeed in managing costs, but are not financially liable to return any money to the payer if they spend more than the target amount.
But ACOs can also take on downside risk. Downside risk models typically offer a higher percentage of the shared savings if the ACO successfully manages costs. However, if the ACO spends more than expected, it is responsible for repaying a portion of the overages back to the payer.
How are healthcare payers and practices putting value-based care into action?
Both commercial and government payers are promoting participation in value-based care with a wide range of programs and options.
The Centers for Medicare and Medicaid Services (CMS) is one of the strongest influences on the development of value-based care. CMS started the Medicare Shared Savings Program also known as MSSP in 2013 to jumpstart the movement to value-based reimbursement models. The MSSP has been highly effective in moving physicians into these arrangements. And the program is continuing to evolve in pursuit of even greater success. In 2019, CMS relaunched the MSSP as “Pathways to Success,” a multi-track system builds on these savings by funneling ACOs into more challenging downside risk arrangements over time.
ACOs that take on risk are eligible for greater rewards within Pathways to Success. In addition, risk-bearing ACOs can take advantage of certain bonuses and exemptions within the Merit-Based Incentive Payment System (MIPS), adding extra encouragement to get involved. Commercial insurers have also been quick to move practices and patients into value-based arrangements. CMS has made it a goal to have all Medicare patients in value-based care by 2030, which will require at least 3 million Medicare beneficiaries to be attributed each year into VBC to reach the goal by 2030. Significant work will need to be done to ensure that we as a specialty are ready for this challenge.
Primary care physicians are leading the way
Physicians who want to take advantage of this growing trend can start by identifying which value-based care options best fit their organization’s clinical and financial goals.
They may also wish to explore the advantages of ACO enablers that can provide the tools and practice transformation advice to help them achieve shared savings and improved patient outcomes.
This combination of quality care and financial incentives will ensure that individuals receive the right care in the right setting at an affordable cost, producing true value for patients, practices, and society as a whole. For family physicians, value-based care may provide the necessary resources to pay for staff bonuses, or extra staffing for care coordination. It is also improving the quality of care patients receive and giving practices insight into data that previously was difficult to obtain.
I have had the privilege of working with many family physicians and others in primary care practices throughout California and the country in value-based care, and it is exciting to see the movement to value based care and the benefits for practices who have made the transition. The quadruple aim of better care at lower cost with improved patient and clinician experience seems closer than ever.
Some tips that I have shared at AAFP FMX and other conferences include but are not limited to the following:
1. The importance of goal setting - set specific, smaller, realistic measurable goals that are time limited, and share the goals with all your staff
2. Review your financial outlook for the year for your practice and diversify income streams, consider value-based care options
3. Evaluate your practice business plan or create one if you don’t have one
4. Understand HCCs and diagnosis documentation - be accurate
5. Know Physician Fee Schedule changes
6. Ensure optimal telehealth strategies and best practices
7. Focus on prevention and follow up e.g. annual wellness visits, transitional care management, review patient access/hours
8. Mark your progress - set a schedule when you will revisit this
9. Get a good partner to help and keep you accountable to help you sustain change, and help you obtain the data required to do optimal VBC work
10. Take steps to recognize burnout, build staff morale, ensure staff safety/PPE - find your ikigai, commit to self-compassion, reframing, gratitude, finding rewarding work and steps to whack the WAC (work after clinic).