Post by Kim Yu, MD, FAAFP
In addition to PPE and testing difficulties, family physicians are seeing declines in patient volumes and record patient cancellations that are completely unprecedented. Practices are seeing declines in patient volume ranging from 30-70%, with many practices dropping by an average of 40-50%. To facilitate telehealth adoption, Aledade supplied practices with a telehealth platform at no cost. All have adopted telehealth rapidly, with 100% of our California practices providing telehealth within 2 weeks, and now seeing increases in volume of telehealth visits to an average of 35-40% of visits (range 20-85%).
Leveraging telehealth is especially important during COVID-19, as patients who require ongoing care are able to access their physicians via telehealth without risking contracting COVID-19. There have been limitations, however, as physicians have reported that many patients are not able to access telehealth because they lack a computer, access to the internet, or smart phones. Some patients lack the ability to navigate the telehealth software. Other platforms, including Facetime, Skype and other services, have helped when difficulties arise with current telehealth platforms, but it is not known how long payers will permit those services.
Parity payments for phone visits that occurred at the end of April were especially helpful to allow for care for the elderly, and those that lacked the technology for true video telehealth visits. Best practice use of telehealth, including scripting for both front office staff, medical assistants and clinicians, patient communication, workflow and implementation, is essential and there are resources available here:
Primary care is not the only place seeing decreased volume. All specialties are seeing declines, with some far more than in primary care (see table) and it is interesting to see how some are trying to address this.
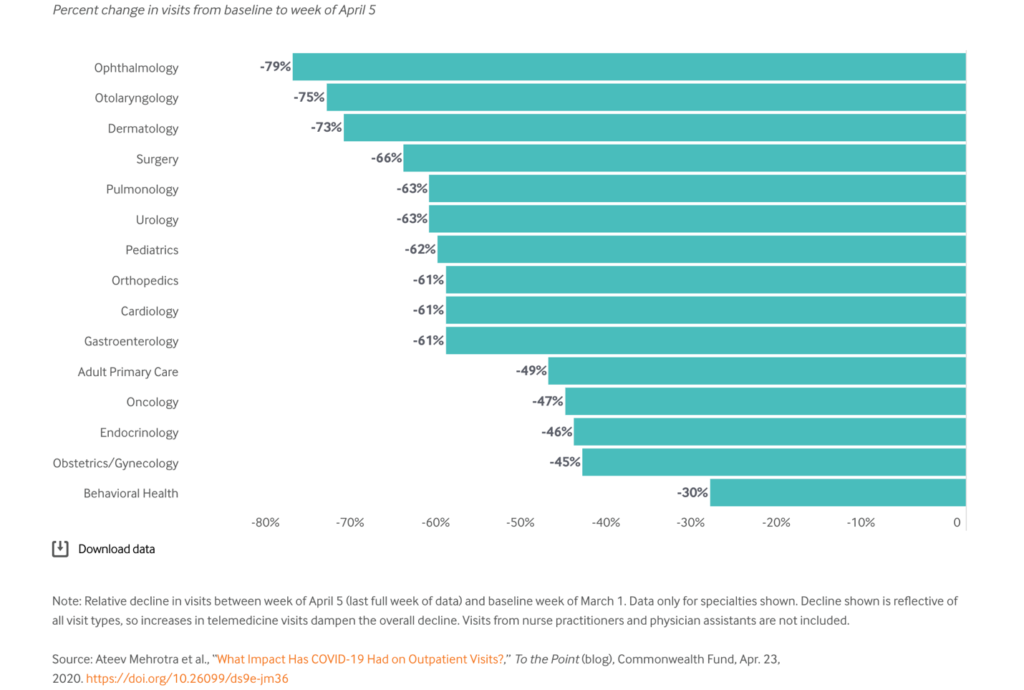
Source: Ateev Mehrotra et al., “What Impact Has COVID-19 Had on Outpatient Visits?,” To the Point (blog), Commonwealth Fund, Apr. 23, 2020. https://doi.org/10.26099/ds9e-jm36 (3)
For those in Emergency Medicine facing declines of 50% or more in volume, one can look at the study done by Adventist Lodi, CA, (4) who found certain interventions helped address patient fears of infection at their ED. In addition to messaging via emails and social media about their cleaning protocols and detailing their pulmonary vs. non pulmonary sectioning pods of their ED, they found that informing patients about risks was important as was providing each patient entering the hospital with a mask, hand sanitizer and wipes. They also provided information on what to expect when arriving at their hospital and alerted patients to what symptoms constitute an emergency.
To ensure patients feel comfortable returning for their visits at their family physician practice, it would be wise to take steps to ensure that all patients are aware of the procedures and steps that your practice has taken for your staff and their safety during this pandemic. This can include car park triage, waiting in cars instead of the waiting room, being escorted directly to patient rooms, converting visits to telehealth visits, especially for those in high risk groups, and informing patients of cleaning procedures, mask usage etc. This information might help alleviate your patients’ concerns of contracting COVID-19 at your practice. Likewise, informing patients of types of visits that may be done via telehealth may help increase patient understanding of what care can be delivered by practices, decreasing the chance that patients will seek out urgent care or emergency department care.
It's important that practices carefully consider ways to increase not only revenue but preventive care as well. If left unchecked, decreased immunization rates may bring severe increases in communicable diseases. Chronic diseases could be left unmanaged to the detriment to patients’ health. On a webinar I spoke at last week, a family doctor from the UK said 2,300 cancer referrals were being deferred in the United Kingdom – each week (5).
To be proactive, consider the following:
References:
3. The Commonwealth Fund - The Impact of the COVID-19 Pandemic on Outpatient Visits: A Rebound Emerges (May 19, 2020)
4. Where Are All the Patients? Addressing Covid-19 Fear to Encourage Sick Patients to Seek Emergency Care, Laura E. Wong, MD, PhD, Jessica E. Hawkins, MSEd, Simone Langness, MD, Karen L. Murrell, MD, Patricia Iris, MD & Amanda Sammann, MD, MPH.
NEJM May 14, 2020 https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0193
5. Cancer Research UK - How coronavirus is impacting cancer services in the UK
6. Telehealth Toolkit Resource link - https://www.aledade.com/covid-19/telehealth